While most psychiatric drugs increase the risk of heat-related illness, authorities warn that individuals taking antipsychotic drugs are at particular risk.
The long, hot days of August can be potentially dangerous for many of the 77 million Americans taking psychotropic drugs, almost all of which increase the risk of heat-related illness, ranging from the mild discomfort of heat cramps to the more serious symptoms of heat exhaustion and life-threatening heat stroke.
Psychotropic drugs can impair the body’s cooling mechanism or cause the people taking them to be less sensitive to signs of overheating, thus predisposing them to heat-related illness. Medical emergencies occur when the body’s temperature rises to dangerous levels and the body becomes unable to lower its temperature. Bodily damage, which can be fatal, occurs if steps are not taken to lower body temperature.

During periods of extreme heat, those taking antipsychotic drugs (also called neuroleptics) are at particular risk of heat stroke, as well as a life-threatening neurological disorder known as neuroleptic malignancy syndrome, according to a recent medical alert from the New York Office of Mental Health. Antipsychotics reduce sweating, the body’s natural means of cooling, as well as reduce the users’ behavior to cool themselves, like drinking more water or removing extra clothing. Even a short time in very hot weather can cause a rapid rise in body temperature for people on these drugs.
Tricyclic antidepressants also decrease sweating, along with inhibiting the body’s ability to regulate temperature, which can result in body temperature rising to dangerous levels during summer heat waves.
Stimulant drugs, like ADHD drugs, are known to raise body temperature, as well as interfere with the body’s ability to cool itself down, so that high summer temperatures can cause body temperatures that are aready elevated by these drugs to go higher still.
Selective serotonin reuptake inhibitor (SSRI) antidepressants can increase sweating while at the same time reducing thirst, which can lead to dehydration and heat illness in very hot weather.
“Due to the lack of research in the field, it is impossible to estimate the scale of the problem.”
– Ying Zhang, senior lecturer, University of Sydney School of Public Health
Research has found that psychotropic drugs increase the risk of heat-related medical emergencies. One study found that those taking antipsychotic drugs have a four times greater risk of admission to a hospital emergency room for heat-related illnesses during a heat wave, while those taking another class of psychiatric drugs, antianxiety drugs, have more than twice the risk of hospitalization. According to the researchers, their results “highlight the negative impact of psychotropic drugs which could interfere with body temperature regulation during heat waves.”
Another study found that taking psychiatric drugs nearly doubles the risk for all causes of death during a heat wave.
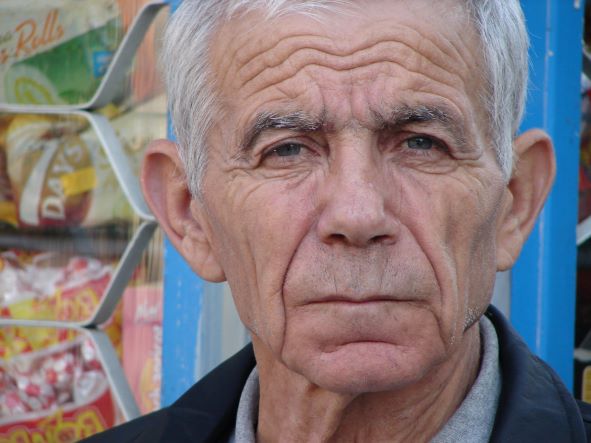
The elderly are even more susceptible to the risk of heat-related illness. The body’s temperature regulation is generally slower in older adults. Compared to young people, older adults also sweat less and radiate less heat, so the core body temperature rises more easily. The rate of hospitalization for heat stroke is significantly higher for older adults and their hospital stays are longer.
How many people taking psychiatric drugs end up with heat-related medical emergencies? Nobody knows.
“Due to the lack of research in the field, it is impossible to estimate the scale of the problem” of the interaction between drugs and heat, Ying Zhang, senior lecturer at the University of Sydney’s School of Public Health, told the Washington Post.
Those taking psychiatric drugs should limit their exposure to summer heat and strenuous activity and drink plenty of water. Seek immediate medical attention for anyone showing signs of heat stroke, including confusion, unconsciousness, a rapid pulse, a high temperature, or red, hot, dry skin.
The Citizens Commission on Human Rights (CCHR) continues to raise awareness of the dangers and the lack of efficacy of psychiatric drugs and practices, which are being reported in a growing body of research studies.
WARNING: Anyone wishing to discontinue or change the dose of any psychiatric drug is cautioned to do so only under the supervision of a physician because of potentially dangerous withdrawal symptoms.
