The proven harm of forced behavioral health treatment raises question of whether the treating psychiatrists violate Hippocratic oath of “first do no harm.”
A new study has found that involuntary hospitalization for substance abuse treatment is not effective, adding to the growing body of research finding that forced behavioral health treatment does more harm than good and raising ethical questions about the use of coercion by the psychiatrists typically in charge of the treatment.
Researchers from Harvard Medical School and Brigham and Women’s Hospital in Boston investigated the outcomes of 22 patients involuntarily committed for substance abuse treatment after first coming to a hospital emergency room. The result was that after release, none of the patients stayed off their alcohol and/or drugs, and all of them ended up in back in the emergency room within a year because of their substance misuse.

“One year following involuntary commitment, all patients had relapsed to substance use and had at least one emergency department visit,” wrote lead author John C. Messinger. Half reverted to substance abuse within two months after the start of their involuntary treatment.
“The study adds to a growing literature recognizing the harms of involuntary commitment for substance use disorder,” the researchers concluded.
Other research has found that forced hospitalization is also ineffective and harmful for mental health treatment. A study earlier this year found no benefit to patients’ mental health condition and no lower risk of death after receiving nonconsensual mental health treatment.
This follows a 2020 study which found that psychiatric in-patients were actually more likely to attempt suicide after release if they were admitted and treated against their will as compared to those who were not.
“The study adds to a growing literature recognizing the harms of involuntary commitment for substance use disorder.”
— John C. Messinger, Harvard Medical School
The harm and lack of benefit from involuntary commitment for psychiatric treatment has resulted in some people avoiding mental health treatment. The U.S. 2011-2019 National Survey on Drug Use and Health revealed that one in four depressed young adults cited their concern over being involuntarily committed to a psychiatric facility or forced to take psychiatric drugs against their will as a reason not to seek mental health treatment.
The potential of involuntary psychiatric hospitalization and treatment doing more harm than good has led some medical professionals to argue that such acts violate the Hippocratic oath of “first do no harm” and should be abolished.
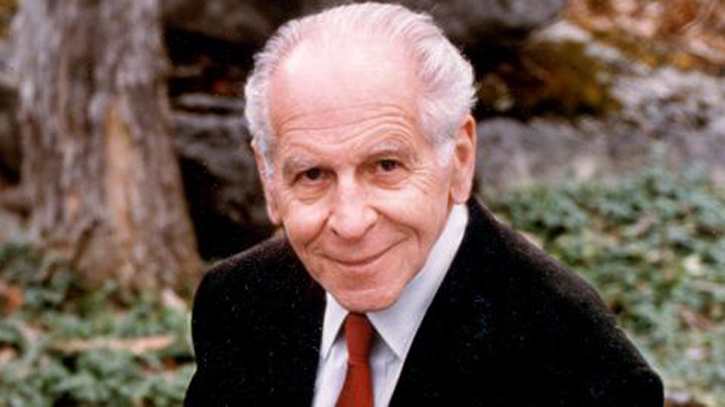
Among them is the co-founder of the Citizens Commission on Human Rights (CCHR), the late professor of psychiatry and humanitarian Thomas Szasz, M.D., who advocated an end to forced psychiatric treatment. Considered by many scholars and academics to be psychiatry’s most authoritative critic, Dr. Szasz wrote: “Increasing numbers of persons, both in the mental health professions and in public life, have come to acknowledge that involuntary psychiatric interventions are methods of social control. On both moral and practical grounds, I advocate the abolition of all involuntary psychiatry.”
The World Health Organization (WHO) has also taken a strong position against coercive mental health practices. In a series of guidelines issued in 2021, WHO stated that nonconsensual practices are used “despite the lack of evidence that they offer any benefits, and the significant evidence that they lead to physical and psychological harm and even death.”
The guidelines further state: “People subjected to coercive practices report feelings of dehumanization, disempowerment and being disrespected. Many experience it as a form of trauma or re-traumatization leading to a worsening of their condition and increased experiences of distress.”
WHO’s call for an end to involuntary mental health treatment extends even to those experiencing acute mental distress. The guidelines note that individuals in mental health crisis “are at a heightened risk of their human rights being violated, including through forced admissions and treatment.”
WHO challenged United Nations member nations, including the United States, to ensure that their mental health services are free from coercion, including forced drugging, the use of physical and chemical restraints and seclusion, electroshock without consent, and involuntary institutionalization.
The Citizens Commission on Human Rights has been a global leader in the fight against the coercive and abusive use of involuntary commitments, seclusion and restraints, psychiatric drugs, and electroshock. In 1969, CCHR issued a Mental Health Declaration of Human Rights that laid out fundamental human rights in the field of mental health to ensure the right to one’s own mind and the right to be free from forced mental health treatment.
