The World Health Organization also cites no proven benefit, but significant evidence of harm from coercive mental health treatment.
Laws permitting involuntary commitment or treatment at a psychiatric facility under certain circumstances are meant to prevent mentally disordered individuals from deteriorating further or harming themselves or others. However, research has not established any clear benefit to psychiatric patients from forced mental health treatment. A new study has also found no benefit to patients in terms of their improved mental health condition or lower risk of death after nonconsensual mental health treatment.
Researchers in Norway analyzed the country’s national health data from 2014-2018 to compare results for adult patients with severe mental disorders who either did or did not receive involuntary treatment at community mental health centers. The centers had either relatively higher or lower rates of involuntary commitments in their designated service areas.

The aim of the study, published in BMC Psychiatry, was to investigate whether there were more harmful outcomes for patients with severe mental disorders in areas with lower rates of involuntary mental health treatment. The researchers hypothesized that if coerced treatment were beneficial, over time there would be worsening mental health conditions and higher rates of suicides and death among patients in areas with lower levels of involuntary treatment compared to areas with higher levels. Those results were not what the researchers found.
“We hypothesized that areas with lower use of involuntary care would show poorer outcomes than areas of higher use. We found no such effect,” wrote the study’s lead author, Olaf Nyttingnes, Ph.D., of the health services research unit at Akershus University Hospital in Norway.
The researchers tested for five possible adverse results and found no statistically significant difference between patients with severe mental disorders who did or did not receive forced mental health treatment. Patients who lived in areas with lower rates of involuntary treatment did not have higher rates of suicide or any-cause mortality, higher rates of inpatient care, or shorter times until an episode of involuntary care, and the number of patients in those areas with severe mental disorders did not increase over time.
“We hypothesized that areas with lower use of involuntary [mental health] care would show poorer outcomes than areas of higher use. We found no such effect.”
— Olaf Nyttingnes, PhD, Akershus University Hospital, Norway
“We did not observe significantly more case fatalities, deterioration into involuntary care, or increases in inpatient days for patients with SMDs [severe mental disorders], nor did we find increased rates of SMDs or notable increases in the numbers of suicides at the area level,” Nyttingnes concluded.
The World Health Organization (WHO) has taken a strong stand against involuntary mental health treatment, in part because of the lack of research finding any benefit to patients. In a series of guidelines issued in 2021, WHO stated that coercive mental health practices are used “despite the lack of evidence that they offer any benefits, and the significant evidence that they lead to physical and psychological harm and even death.”
WHO advised United Nations member nations, including the United States, to take bold steps to ensure that their mental health services are free from coercion, including forced drugging, the use of physical and chemical restraints and seclusion, electroshock without consent, and involuntary institutionalization.
WHO’s call for an end to involuntary mental health treatment extends to those experiencing acute mental distress. The guidelines note that individuals in mental health crisis “are at a heightened risk of their human rights being violated, including through forced admissions and treatment…. These practices have been shown to be harmful to people’s mental, emotional and physical health, sometimes leading to death.”
WHO’s rejection of nonconsensual mental health treatment echoes the long-time advocacy of the Citizens Commission on Human Rights (CCHR) to end involuntary treatment and harmful psychiatric practices and restore human rights and dignity to the field of mental health.
“People subjected to coercive practices report feelings of dehumanization, disempowerment and being disrespected,” according to the WHO guidelines. “Many experience it as a form of trauma or re-traumatization leading to a worsening of their condition and increased experiences of distress.”
The WHO guidelines lay out a vision of holistic mental health services, as contrasted with today’s narrow focus on the diagnosis and drugging of individuals to suppress symptoms, a mental health approach that results in “an over-diagnosis of human distress and over-reliance on psychotropic drugs.”
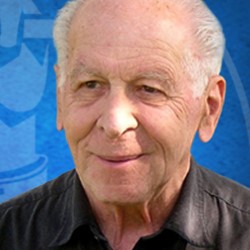
Years ahead of the WHO reports, CCHR’s co-founder, the late professor of psychiatry and humanitarian Thomas Szasz, M.D., advocated an end to forced psychiatric treatment. Considered by many scholars and academics to be psychiatry’s most authoritative critic, Dr. Szasz wrote: “Increasing numbers of persons, both in the mental health professions and in public life, have come to acknowledge that involuntary psychiatric interventions are methods of social control. On both moral and practical grounds, I advocate the abolition of all involuntary psychiatry.”
As a human rights organization and mental health industry watchdog, the Citizens Commission on Human Rights has exposed and campaigned against the abusive use of involuntary institutionalization and psychiatric treatments given without consent, including forced drugging, restraints, and involuntary electroshock. CCHR’s Mental Health Declaration of Human Rights enumerates the rights we believe each individual is entitled to in the mental health system.
